JDO Vol. 58
Editorial
Dr. Chris H. Chang
Recently I was invited to speak at the AAO Mid-Winter Meeting and was honoured to have been on the stage with the world’s best 20 open-bite speakers. The organizer, Professor Greg Huang from the University of Washington, issued a specific format and several guidelines as to how he wished each speaker to present - 45 minutes in length, structured with Introduction, Literature, Case Report and Conclusion sections.
This is all well and good, but I couldn’t help wondering if we are actually being constrained by such strict guidelines…
Correction of Generalized Interdental Spacing, Gummy Smile and Implant Site Development with Invisalign®
Eric Hsu, Chris H. Chang, W. Eugene Roberts
Abstract
A 30-year-old male presented with a Class I malocclusion: congenitally missing lower lateral incisors, generalized anterior spacing in both arches, and a gummy smile. Motivation for orthodontic consultation was smile improvement without wearing braces. Clear aligners were used to retract the maxillary incisors, close upper anterior spaces, and prepare implant sites to restore the missing lower lateral incisors. Retraction of the maxillary incisors was associated with a relative intrusion of the central incisors to improve the gummy smile. After 26 months of aligner treatment, the patient declined further refinement to improve axial inclinations because he was satisfied with the results. Overall, a malocclusion with a Discrepancy Index of 10 was corrected to a Cast-Radiograph Score (CRE) of 12, with a Pink & White dental esthetic score of 5. (J Digital Orthod 2020;58:4-18)
Key words: Invisalign®, aligner treatment, gummy smile, spacing, congenital missing lower incisors, implant site preparation, second order tooth movement
Download Article
Class II Malocclusion with Blocked-Out Maxillary Canines and a Steep Mandibular Plane:
Non-Extraction Treatment with 5-Year Follow-Up
Lexie Y. Lin, Jennifer Chang, Kristine Chang, W. Eugene Roberts
Abstract
History: A 10-year-old female was referred because of bilateral unerupted maxillary canines.
Etiology: Insufficient arch perimeter resulted in the premature loss of the upper deciduous canine (Uc) space due to ectopic eruption of adjacent maxillary lateral incisors.
Diagnosis: Increases in lower facial height (56%), mandibular plane angle (SN-MP 40.5 ̊), intermaxillary relationship (ANB 4 ̊), and lip protrusion (1mm/2mm to the E-Line) were associated with full cusp Class II molar relationships, bilaterally. Both upper canine spaces were lost due to tipping of adjacent teeth into the exfoliated Uc spaces, and the upper left first premolar (UL4) was rotated mesial-in. The upper right canine (UR3) was well positioned, but its path of eruption was blocked. The UL3 was high in the alveolar process and at risk for impaction. The maxillary arch perimeter was deficient (-8mm) due to premature loss of upper deciduous canines, but no significant root resorption was apparent. The American Board of Orthodontic (ABO) Discrepancy Index (DI) was 25.
Treatment: A full fixed passive self-ligating (PSL) appliance was bonded on all permanent teeth. Compressed coil springs were inserted to open space and the maxillary canines erupted spontaneously. Intermaxillary growth helped correct the Class II molar relationship as the canines erupted, and the occlusion was finished with vertical elastics. Retention was with clear aligners.
Outcomes: After 27 months of active treatment, the blocked-out maxillary canines were well aligned. The supporting gingiva was healthy, periodontal form was near ideal, and no root resorption was noted. Final alignment and dental esthetics were excellent as evidenced by an ABO Cast-Radiograph Evaluation (CRE) score of 18, and an International Board of Orthodontics and Implantology (IBOI) Pink & White Esthetic Score of 3. Follow-up records 5 years later documented the stability of the correction.
Conclusions: The etiology of a blocked-out canine indicates the most efficient timing for orthodontic intervention. Space maintenance is indicated if an Uc is lost due to ectopic eruption of the lateral incisors. Otherwise adjacent teeth may drift into the canine space preventing normal eruption of the permanent cuspid(s). Phase I treatment is required to prevent ectopic buccal eruption or impaction. (J Digital Orthod 2020;58:24-39)
Key words: Impacted maxillary canine, eruption, etiology, ectopic eruption, spontaneous correction, Class II malocclusion
Download Article
Non-Extraction Treatment of a Class III/Class I Malocclusion with Anterior Crossbite
Charlene Chang, Angle Lee, Chris H. Chang, W. Eugene Roberts
Abstract
History: No contributing medical factors were reported, but ectopic eruption of the maxillary central incisors was probably an etiologic factor for the anterior crossbite.
Diagnosis and Etiology: Ectopic eruption of the maxillary central incisors was deemed the proximal cause of this asymmetric malocclusion (Class III right, Class I left) with 1.5mm midline discrepancy and anterior crossbite. There was about a 1mm functional shift (forward and left), and the 3-ring diagnostic sequence indicated conservative management was feasible.
Treatment: Correct anterior crossbite with an anterior bite turbo and early light short elastics. Interproximal enamel reduction in the lower arch is needed. Retract the mandibular arch with mandibular buccal shelf (MBS) bone screw anchorage.
Results: The anterior crossbite was corrected in 4 months, but lower arch retraction and finishing required 21 months of active treatment. Upper lip protrusion and lower lip retrusion improved the facial profile. The Cast-Radiograph Evaluation (CRE) was 15, and the Pink & White Esthetic Score was 3.
Conclusions: Conservative anterior crossbite correction combined with retraction of the entire lower arch produced stable facial and dental outcomes four years after treatment. (J Digital Orthod 2020;58:46-64)
Key words: Class III/Class I malocclusion, anterior crossbite, bite turbo, early light short elastics, interproximal reduction, MBS bone screws
Download Article
Simplified Removal of an Osseointegrated Implant for Space Closure to Correct Anterior Crossbite
Linda Tseng, Chris H. Chang, W. Eugene Roberts
Abstract
Diagnosis: A 45-year-old male presented for orthodontic consultation with concerns about a concave facial profile and anterior crossbite. Clinical examination showed facial asymmetry with a cant in the occlusal plane that was associated with mandibular deviation to the right by about 2mm. Cephalometrics revealed a skeletal bimaxillary protrusion (SNA 89°, SNB 89°, ANB 0°). There were multiple missing teeth (UR8, UR7, UR4, UL2 , UL8, LR6, LL6, and LL8), and four endodontically treated teeth (UL5, UL7, LR7, LL6, and LL7). Missing lower first molars were restored with a fixed prosthesis on the right side and an implant-supported prosthesis on the left. A large area of pathology, possibly condensing osteitis, was distal and apical to the root of the LL4.
Treatment: All restorations were replaced by provisional crowns except for the metal crown on the UL7, and the gold crown on the LL8. The pontic restoring the LR6 was cut out with a handpiece. An osseointegrated implant-supported prosthesis (ISP) restoring the LL6 was removed with a sustained counterclockwise torsional load (see text for details). A passive self-ligated, fixed appliance with anterior bite turbos (UR1, UL1) was used to correct the anterior crossbite by retracting the anterior segment with space closure mechanics, supplemented with light force Class III elastics. The edentulous space for the UR4 was opened with a compressed coil spring to receive an ISP. After orthodontic treatment, all provisional crowns were restored with porcelain fused to metal (PFM) prostheses.
Results: After 38 months of treatment, the profile was improved, midlines were coincident, and normal overjet/overbite was achieved. The anterior crossbite was corrected and molar relationships were Class II on the left and Class I on the right. Lower incisors were tipped distally (76.5°), and upper incisors were flared labially (116°). All prostheses were restored as needed. The apparent condensing osteitis apical to the root of the LL4 decreased in size and remained asymptomatic, but endodontic evaluation is indicated. A complex malocclusion with a Discrepancy Index (DI) score of 19 was treated to a Cast Radiograph Evaluation (CRE) of 13.
Conclusions: Osseointegrated implants can be easily removed with a simplified torsional overload procedure to permit optimal orthodontic management of malocclusion. (J Digital Orthod 2020;58:68-90)
Key words: Implant removal, anterior crossbite, minimally invasive approach, space closure
Download Article
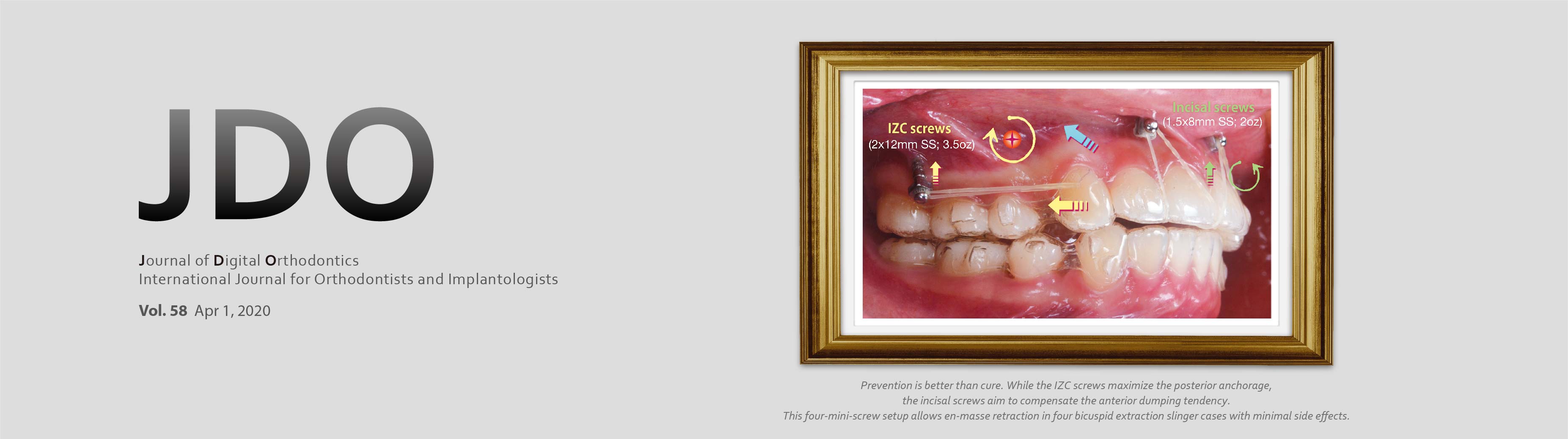
Mechanics and Clinical Significance for Mini- Screws in Four-Bicuspid Extraction Aligner Cases
Lexie Y. Lin, Chris H. Chang, W. Eugene Roberts
Abstract
When treating extraction cases with clear aligner therapy, root paralleling during space closure has been inconsistently. Even the G6 (Align Technology, Inc., San Jose, CA, USA) solution does not guarantee highly predictable tooth movement. Anchorage loss and unwanted side effects are still encountered. The aim of the present article is to propose a mini-screw gold standard of care for patients who demand inconspicuous aligner therapy involving extraction of four first premolars. (J Digital Orthod 2020;58:94-98)