JDO Vol. 74
Editorial
Chris H. Chang
Reflections on Visiting Machu Picchu, Peru
This year in February, I was invited to give an orthodontic lecture for a day in Lima, Peru. Having concluded the lecture, I visited Machu Picchu, arguably the most famous ancient Inca icon in Peru. Even though it lies only 230 km away from Cusco, it was in fact a full-day venture, taking us from 4:00am until 10:00pm. However, despite the amount of time required, we actually only spent just over an hour exploring it. Furthermore, as a cultural heritage site, there are no restroom facilities inside, and visitors must pay one US dollar to use the restroom before entering.
If someone asked me whether Machu Picchu was worth visiting or not, my answer would be that yes, it is certainly worth visiting, but it’s not worth enduring such an arduous ordeal. My wife questioned that if that were the case, why would so many people find this mysterious place worth visiting? My response is that it is a lost city from five hundred years ago and was discovered completely intact and with no existing records since the Inca Empire had not established a writing system. It’s hard for me to imagine an Empire without a writing system…
Common Complications in Orthodontic Bone Screws: Causes, Management, and Prevention
Vicky T. Huang, Chris H. Chang, W. Eugene Roberts
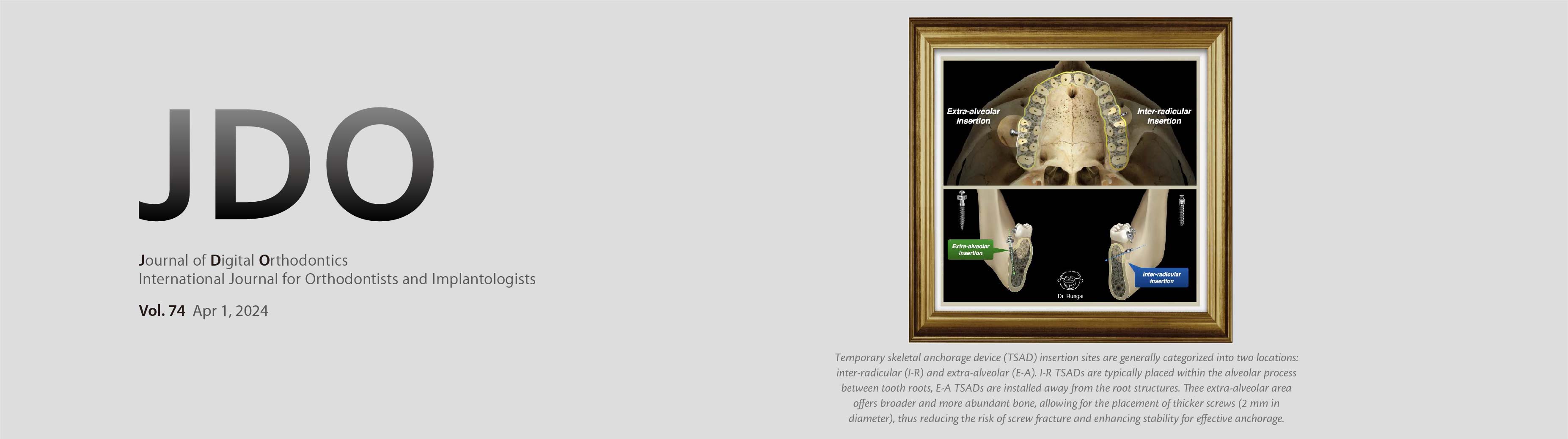
Orthodontic bone screws, also known as temporary skeletal anchorage devices (TSADs), have significantly expanded the possibilities in orthodontic treatment. However, like any orthodontic intervention, complications can arise. This article examines three common complications associated with TSADs: soft tissue damage, hard tissue damage, and screw fracture. We explore the causes, management strategies, and preventive measures for each of these issues.
Non-Extraction Treatment and Correction of Generalized Interdental Spacing and Protrusive Anterior Teeth in an Adolescent
Ping-Hsuan Yeh, Chris H. Chang, W. Eugene Roberts
Introduction: A 10-year-11-month-old female was brought by her mother to seek orthodontic consultation, with a chief complaint of a protrusive lower lip.
Diagnosis: Cephalometric analysis revealed a skeletal Class I relationship (SNA, 83°; SNB, 81°, ANB, 2°), protrusive lower lip, as well as proclined upper and lower incisors. An intraoral assessment revealed mild Class II canine relation on the right side. There were slight generalized spaces in the upper and lower dentition. The Discrepancy Index (DI) was 10.
Treatment: The treatment plan was a non-extraction treatment using Damon® brackets anchored with infrazygomatic crest (IZC) bone screws bilaterally to retract the upper and lower dentitions. The active treatment time was 23 months.
Results: Improved dentofacial esthetics and a better occlusal function were achieved after treatment. The Cast-Radiograph Evaluation (CRE) was 13, and Pink and White esthetics score was 9. The patient was well satisfied with the final outcome.
Conclusions: IZC bone screw serve as an excellent anchorage in the treatment which molar protraction is undesirable. (J Digital Orthod 2024;74:18-30)
Key words: lower lip protrusion, generalized spacing, IZC screws, anchorage
Download Article
Non-Extraction Treatment of a Class II Openbite with Amelogenesis Imperfecta
Yu-Hsin Huang, Kim-Coy Low, Po-Jan Kuo, John Jin-Jong Lin, W. Eugene Roberts
Introduction: A 15 year-7 month-old female with a history of amelogenesis imperfecta (AI) presented with chief complaints of poor dental esthetics and anterior openbite.
History and Etiology: AI is a hereditary disorder that is usually manifested as an autosomal dominate trait involving defective ENAM gene(s). For the present patient, deficient enamel resulted in decreased biologic width of the epithelial attachment, in addition to dental attrition that reduced the heights of clinical crowns. Selective crown lengthening and complete provisional restoration were required. Habitual interdental tongue posture, which may reflect a history of airway compromise, resulted in an anterior openbite that induced posterior mandibular rotation to produce a long face.
Diagnosis: AI-related enamel deficiency has compromised the periodontium and dentition. Facial form was convex (12°) with increased lower facial height (59.5%) and a steep mandibular plane angle (FMA, 37.5°). Cephalometrics revealed a protrusive maxilla (SNA, 84.5°), retrusive mandible (77.5°), and an intermaxillary discrepancy of 7° (ANB). The bilateral Class II malocclusion was complicated with anterior openbite, canted occlusal plane, and mandibular deviation to the left. The Discrepancy Index (DI) was 62.
Treatment: Crown lengthening surgery and revised provisional restorations established a healthy periodontium in preparation for orthodontics treatment. A fixed passive self-ligating appliance, with high torque brackets in the upper anterior segment, was bonded on both arches. Anchorage to intrude upper molars was provided with bilateral infra-zygomatic crest (IZC) bone screws. After initial orthodontic alignment, interproximal space was increased as needed with elastic separators to prepare gingival margins, and a new set of optimized provisional restorations was fabricated. Orthodontic finishing was accomplished with the same fixed appliance.
Results: Crown lengthening produced healthy periodontium with proper biological width in preparation for full provisional restoration and orthodontic alignment. As upper molars were intruded, the mandible rotated anteriorly, and the lower facial height decreased as lip and chin protrusion increased. This challenging openbite malocclusion, with a Discrepancy Index (DI) of 62, was treated in 22 months to an excellent outcome: Cast-Radiography Evaluation (CRE) score of 11 and Pink & White dental esthetic score of 1. An upper removable retainer was provided for night-time wear.
Conclusions: A patient with AI and an anterior openbite malocclusion was treated to a stable occlusion with a passive self-ligating fixed appliance and IZC bone screw anchorage. Interdisciplinary treatment with periodontics and prosthodontics was required before and after orthodontic therapy to appropriately restore dentofacial esthetics and function. (J Digital Orthod 2024;74:38-58; reprinted from J Digital Orthod 2020;57:4-23)
Key words: Class II, openbite, occlusal cant, bimaxillary protrusion, molar intrusion, infrazygomatic crest screw, amelogenesis imperfecta, therapeutic provisional restoration
Download Article