JDO Vol. 59
Editorial
Dr. Chris H. Chang
This year saw a new development in the AAO history – the first ever virtual annual meeting. It was a great honor to kick off this event, and an even greater honor to have received a 99.7% approval rating from my peers.
I have had time during the COVID-19 recess to assess many things to help improve my professional skills. One avenue that I contemplated was my presentation timeline, starting in 2009 up until the aforementioned virtual meeting. I was most touched by a comment that Melissa McCulloch, the Education Specialist of AAO, kindly pointed out to me that my “wisdom and skill are most valuable and directly transferable to clinical practice and life…
Partially Edentulous Asymmetric Class III Malocclusion: Lower Second Molar Extraction, Autotransplantation, and Space Closure
Eric Hsu, Po-Jan Kuo, John Jin-Jong Lin, W. Eugene Roberts
Abstract
Diagnosis: A 34-year-7-month-old female presented with chief complaints of compromised facial esthetics and unilateral collapse of posterior occlusion. Clinical examination revealed mandibular prognathism, facial asymmetry, Class III malocclusion, missing LL6, residual roots of LL7 and LL8, and over eruption of UL5-UL7. The Discrepancy Index (DI) was 25.
Treatment: A conservative treatment plan was designed to preserve the natural dentition. To create a symmetric occlusal plane, the UL5-UL7 segment was intruded with anchorage provided by two 2x8-mm mini-screws. The LR7 was endodontically treated and autotransplanted into the LL7 extraction socket. A passive self-ligating appliance was installed to align and retract the lower dentition to correct the Class III molar relationship.
Outcomes: The autotransplanted molar healed successfully, and subsequently ankylosed in an acceptable position. The bite was opened about 1.5°, crowding was corrected, and the dentition was well aligned to Class I canine and molar relationships. The ABO Cast-Radiograph Evaluation (CRE) was 22, and the Pink & White dental esthetics score was 7. (J Digital Orthod 2020;59:4-19)
Key words: Autotransplantation, Class III malocclusion, increased vertical dimension of occlusion, molar intrusion, facial asymmetry, mandibular arch retraction
Download Article
Surgical Procedures, Mechanics, and Problems in Recovering 51 Impacted Maxillary Canines for 46 Patients with the OBS-3D Lever Arm Appliance
Chris H. Chang, Eric Hsu, W. Eugene Roberts
Abstract
Objective: Assess recovery for consecutive impacted maxillary canines (I-U3s).
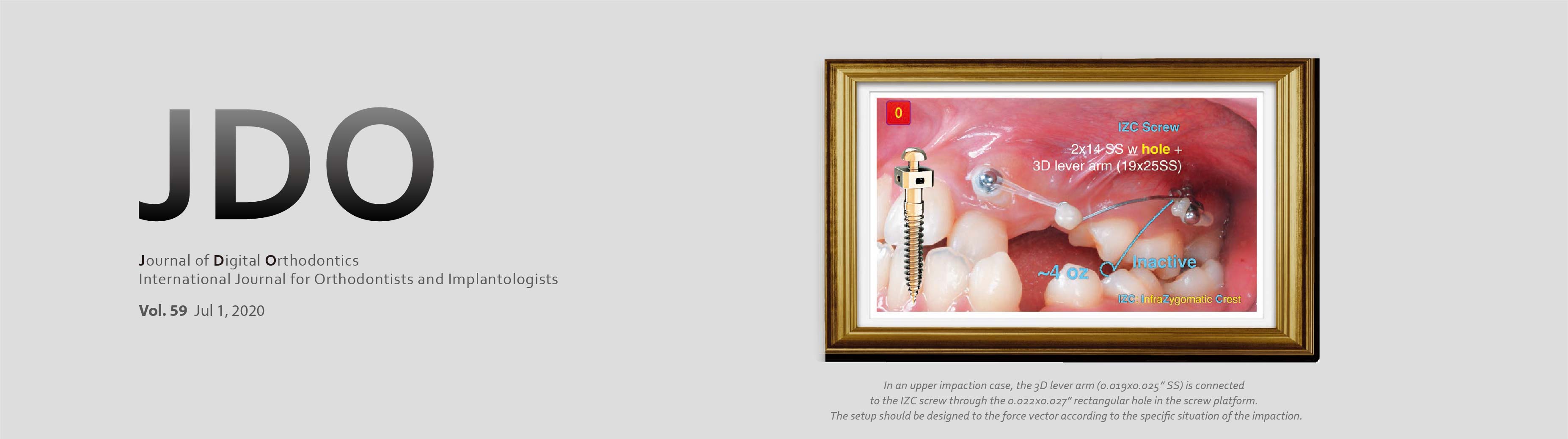
Materials and Methods: Based on three-dimensional (3D) imaging, 51 I-U3s were recovered from 46 patients: 11 male, 35 female, mean age 16.5 years (range 10-36 yr). Orthodontics prepared a path for movement of the I-U3s as needed. Minimally invasive surgery uncovered the I-U3s and removed bone to the level of CEJ. 3D anchorage was provided with a 2mm diameter stainless steel (SS) OrthoBoneScrew® (OBS). A rectangular slot secured a custom SS wire segment (OBS-3D lever arm) to align the I-U3.
Results: Impaction locations were according to side (22 right, 29 left), and surface (32 labial, 19 palatal). I-U3s were optimally aligned in an average of 11.7 months (M), but six more severe labial impactions required up to 17M, and six complete transpositions required 27-30M. Moderate root resorption (<2mm) on the adjacent lateral incisor was noted for four I-U3s (3 labial, 1 lingual). Gingival recession affected 19 recovered canines (11 labial, 8 palatal); all were moderate (Miller Class I) except for one severe problem (Miller Class III).
Conclusions: The OBS-3D lever arm is a biomechanic system that enhances the probability of success by controlling treatment duration and complications. Root resorption on adjacent lateral incisors is best avoided by not bonding a bracket on them during the recovery process. (J Digital Orthod 2020;59:24-33)
Key words: Maxillary canine, impaction, transposition, bone screw, 3D lever arm, gingival recession, root resorption
Download Article
Extraction Treatment for a Class I Malocclusion with Bimaxillary Crowding and Deep Overbite
Lomia Lee, Chris Lin, Chris H. Chang, W. Eugene Roberts
Abstract
A 23-year-1-month-old male presented for orthodontic consultation to evaluate crowding and facial protrusion. Clinical examination revealed a lower lip protrusion, increased facial height (58.5%), retrusive jaws (SNA 79.5°, SNB 74.5°), Class I molar relationship, bimaxillary crowding, flared incisors (U1 to SN 110°, L1 to MP 106°), excessive Curve of Spee, and deep overbite. The ABO Discrepancy Index (DI) was 21. All four first premolars were extracted and the malocclusion was treated with passive self-ligating brackets, sliding wire space closure, and auxiliary root torquing springs. Treatment outcomes are documented with an ABO Cast-Radiograph Evaluation (CRE) of 27 and a Pink & White (P&W) dental esthetic score of 4. (J Digital Orthod 2020;59:40-57)
Key words: Crowding, deep overbite, torque control, passive self-ligating brackets, auxiliary root torquing (ART) spring
Download Article
Efficient Procedure for Precise Bonding of Aligner Attachments
Joshua Lin, Chris H. Chang, W. Eugene Roberts
Abstract
Computer-generated attachments, as specified in the ClinCheck® simulation, must be precisely duplicated chair-side on the patient’s dentition. This article describes the use of flexible attachment templates for each quadrant. Windows (reliefs) for each specified attachment are filled with composite resin that is bonded on the surface of the teeth. Standard operative procedure, quality control checks, and patient training are reviewed. This article provides step-by-step descriptions and illustrations for efficiently and precisely initiating aligner therapy. This protocol is standard operating procedure at the Beethoven Orthodontic Center. (J Digital Orthod 2020;59:64-73)
Towards a Contemporary and Reasoned Orthodontics: An Interview with Dr. Chris Chang
Stéphane Renger
This interview was conducted by Dr. Stéphane Renger before Dr. Chang’s lecture in the annual Prestige Day of the French Society of Dento-Facial Orthopedics (SFODF) and was originally published in the Journal of French Orthodontics (L’Orthodontie Française) in 2018 in French. It was translated to English by Dr. Stéphane Renger and reprinted with permission. (J Digital Orthod 2020;59:78-88)